CYSTIC FIBROSIS
In Mexico every year there are 350 new cases of cystic fibrosis. Neonatal screening is a test to detect this disease before symptoms appear. However, this is not a confirmatory test and does not detect cystic fibrosis in all patients. In addition, it is important to know what mutation is presented for adequate treatment through other molecular tests. Cystic fibrosis must be detected and treated from the first days of life, since patients without adequate treatment can die during childhood or adolescence.
At Genolife we carry out different molecular tests that can help you with an early detection of the disease. Here we mention what they are and we can guide you on which one to choose.
What is cystic fibrosis?
Cystic fibrosis (CF) is an autosomal recessive disease that occurs in approximately 1/3,500 births. Most patients become symptomatic at or shortly after birth, with respiratory infections and poor weight gain being the most common symptoms.
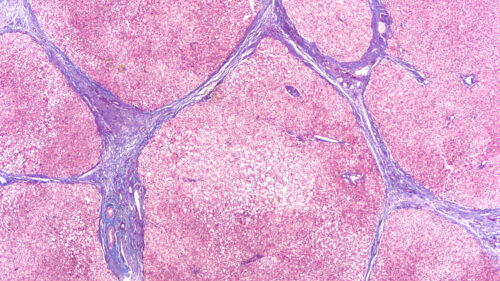
Cystic fibrosis is a multisystem disease that affects the epithelium of the respiratory tract, pancreas, intestine, hepatobiliary system, and exocrine sweat glands. Morbidities arising from cystic fibrosis include progressive obstructive pulmonary disease with bronchiectasis, frequent hospitalizations for pulmonary disease, pancreatic insufficiency and malnutrition, recurrent sinusitis and bronchitis, and male infertility. Lung disease is the leading cause of morbidity and mortality in cystic fibrosis.
In recent years, remarkable improvements have been seen in the health of people with cystic fibrosis, life expectancy has increased substantially, however, this disease still continues to limit survival and quality of life in people who suffer from it.
The symptoms and signs that can be found in children and young adults are:
- Salty taste of the skin, they can have two to five times more salt in their sweat
- Intestinal obstruction
- Pancreatic insufficiency that usually manifests in the first stages of life and that can be progressive
- thick mucus
- Chronic or wheezing cough
- Frequent respiratory infections producing pneumonia and bronchitis
- Nasal polyps and chronic sinusitis
- Inflammation and obstruction of the bile ducts
- Displacement of one part of the intestine within the other
- Adolescents may experience growth retardation, delayed onset of puberty, and decreased exercise tolerance
- Danger of dehydration in feverish periods due to excessive sweating
What causes this disease?
We have known since 1989 that CF is caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene that encodes the CFTR protein. This anion channel, which conducts chloride and bicarbonate in the apical membrane of different epithelia, regulates the transport of water and ions, and maintains the hydration of the epithelial surface.
The release of bicarbonate in the respiratory tract is important for the correct development of mucins and defense against bacteria. In the intestine, the release of bicarbonate is needed to buffer gastric acidity and allow activation of pancreatic enzymes. So far, more than 2,000 different CFTR mutations have been reported, and F508del is by far the most common.
Diagnosis of the disease
Neonatal screening and chlorine in sweat
Cystic fibrosis is now recognized as a major genetic disease throughout the world. The diagnosis is made mainly through the CF Neonatal Screen.
The CF neonatal screen identifies high levels of immunoreactive trypsinogen (IRT) in the newborn’s blood. It is not a diagnostic test, so a positive result requires confirmation with diagnostic tests: chlorine in sweat or molecular study.
Being alert to CF remains important, because neonatal screening does not detect CF in all patients and the disease may only manifest in adulthood. In addition to the fact that it is essential to carry out a molecular study since knowing what the patient’s CFTR mutations are opens the way to personalized therapy.
molecular tests
The discovery of the CF gene regulator (CFTR) has transformed the lives of CF patients by leading to a treatment that can prevent major complications if started early in childhood or as early as possible in the patient .
At Genolife we have the following studies to help with a timely diagnosis of Cystic Fibrosis in patients suffering from the disease or in patients suspected of being carriers of the related gene:
Single gene testing (detection of point mutations)
This test is performed primarily for the diagnosis of CF by targeted analysis for pathogenic CFTR variants.
Note:
-The panel recommended by the American College of Medical Genetics includes all 23 pathogenic variants and has a detection rate of 97% in Eastern European Jews, 88.3% in non-Hispanic whites, 69% in African Americans, and 57% in Hispanic Americans; The detection rate in Asian Americans is unknown.
-A panel that includes more than 129 pathogenic variants would detect approximately 96% of the pathogenic variants in affected individuals.
Complete Sequencing of the CFTR Gene by NGS
CFTR sequence analysis, followed by gene-directed deletion/duplication analysis, is performed if only one pathogenic variant or none are found.
Note:
It is the initial diagnostic test for:
-Individuals of an ethnic group for whom the sensitivity of targeted analysis is low.
-Prenatal testing in a high-risk fetus.
-Prenatal testing in a low-risk fetus with echogenic bowel identified on a prenatal ultrasound examination.
-A baby with an elevated IRT test at newborn screening and a sweat chloride of 30-59 mEq/L (intermediate result).
-A symptomatic baby (eg, baby with meconium ileus) who is too small to produce adequate volumes of sweat.
Multigene panel
It includes the CFTR gene and other genes of interest. In the gene panel, chosen genes are studied, genes that we already know that if they are mutated they can cause one disease or another.
Note:
– The gene panel allows us to study many genes at the same time, and in most cases a mutation causing the disease suffered by the patient is detected. In cases where no mutation is detected, exome study is advisable to determine which gene is mutated in the patient.
Exome sequencing
The study of the exome allows us to know which mutations are found throughout the genome. It is a powerful tool that allows us to analyze our genetic code in depth, since its objective is to obtain the maximum genetic information possible from a patient, looking for genetic variants throughout the approximately 20,000 genes that constitute it.
One of the greatest advantages of this technique is that it helps us to accurately detect any genetic alteration that could have a direct impact on our quality of life.
Although its cost is higher, it provides us with much more information than the previous ones, since it allows the detection of variants related to this disease and others. Sometimes it is more expensive to carry out individual tests to have an accurate diagnosis of the disease and this test can save us from the famous diagnostic odyssey.
Important points
- Improved molecular genetic diagnostics have allowed identification of cystic fibrosis and also in individuals with nonclassical presentations of fibrosis and related disorders.
- Defining the mutations present in the CFTR gene associated with disease manifestations is a priority to guide patient follow-up and treatment decisions.
- There is no definitive cure for Cystic Fibrosis, however, the FDA has approved medications that consist of a combination of compounds that, on the one hand, increase the amount of CFTR protein on the cell surface and, on the other hand, increase the function of the protein. The use of drugs for certain mutations in the CFTR gene responsible for cystic fibrosis has also been approved.
Bibliography
- Bell, S. C., Mall, M. A., Gutierrez, H., Macek, M., Madge, S., Davies, J. C., … & Ratjen, F. (2020). The future of cystic fibrosis care: a global perspective. The Lancet Respiratory Medicine, 8(1), 65-124.
- Boucher RC. An overview of the pathogenesis of cystic fibrosis lung disease. Adv Drug Deliv Rev 2002; 54:1359–71.
- De Boeck, K. (2020). Cystic fibrosis in the year 2020: A disease with a new face. Acta paediatrica, 109(5), 893-899.
- De Boeck K, Vermeulen F, Dupont L. The diagnosis of cystic fibrosis. Presse Med 2017; 46:e97–108. 3.
- Goetz D, Ren CL. Review of Cystic Fibrosis. Pediatr Ann 2019; 48:e154–61.
- Kunzelmann K, Schreiber R, Hadorn HB. Bicarbonate in cystic fibrosis. J Cyst Fibros 2017; 16:653–62.
- Mehta, G., Macek Jr, M., Mehta, A., & European Registry Working Group. (2010). Cystic fibrosis across Europe: EuroCareCF analysis of demographic data from 35 countries. Journal of Cystic Fibrosis, 9, S5-S21.
- Quinton PM. Cystic fibrosis: impaired bicarbonate secretion and mucoviscidosis. Lancet 2008; 372:415–
- Shah VS, Meyerholz DK, Tang XX, Reznikov L, Abou Alaiwa M, Ernst SE, et al. Airway acidification initiates host defense abnormalities in cystic fibrosis mice. Science (80- ) 2016; 351:503–7.
- Ong, T., Marshall, S. G., Karczeski, B. A., Sternen, D. L., Cheng, E., & Cutting, G. R. (2017). Cystic fibrosis and congenital absence of the vas deferens.
- Cystic Fibrosis Mutation Database [Internet]. Available from: http://www.genet.sickkids.on.ca